Running Assessment
Gait Analysis, or simply, a running assessment is studying how we walk or run. We use this to identify and diagnose gait disorders. Athletes and active individuals, people with musculoskeletal conditions, and individuals dealing with injuries in the lower limbs are people who should be seen to do a running assessment.
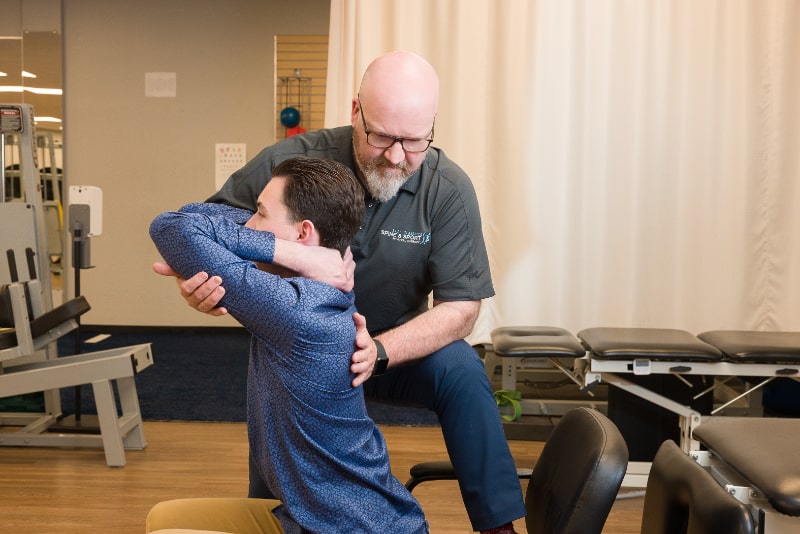
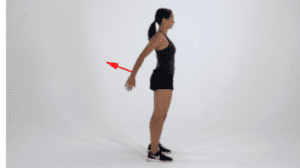
At East TN Spine & Sport, our running assessment begins with talking to our patients about their current training program–if any, running shoes and surface, running goals and aspirations, and current or previous history of injury. This is then followed by having our patients warm up on the treadmill until they reach a comfortable speed. A therapist will videotape their patients running on the treadmill, capturing views from both the side and the back. Using slow-motion software, we are able to watch the replay of our patients running frame-by-frame. This allows us to look closely at where our patients are landing, how they are landing, and any other biomechanical misalignments. At the conclusion of your gait analysis, your therapist will make recommendations to address issues that may be causing your pain/injury or to maximize your running efficiency.
Examples of training recommendations that may be made following your running assessment include:
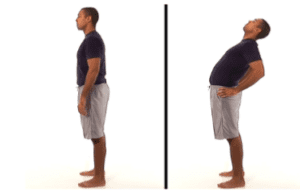
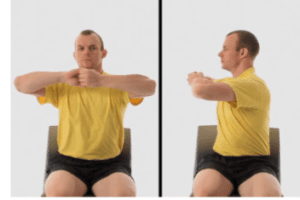
- Hip strengthening or core exercise program to address excessive pelvic movement while running that could lead to hip or knee pain
- Landing drills to address runners who land too hard while running that could cause stress injuries
- Recommendations for shoes or inserts in addition to foot strengthening exercises to address excessive foot movement (pronation or supination ) while running that could cause ankle pain or tendinitis
- Cadence training using a metronome to address runners who take longer strides leading to heel striking which could increase force while running and cause injuries from the ankle to the hip.
Some of our locations provide the AlterG anti-gravity treadmill, this treadmill is mainly used to shorten recovery times, reduce injury, and improve mobility for patients. Using its weight-reducing ability, The AlterG anti-gravity treadmill was designed to return to walking after injury, surgery, or pain sooner than before while still walking or running normally. Our AlterG Treadmills also provide gait analysis. Locations that offer this NASA technology include Hardin Valley, Farragut, and Oak Ridge.