By Taryn Bader Pelvic Health, Therapy back pain, constipation, female, menopause, pain, pelvic floor, pelvic health, pelvic pain, physical therapy, puberty, Therapy, urinary incontinence, urination, vagina, Women Women experience continuous changes throughout their lifespan; from puberty to childbearing years, perimenopause, and into postmenopause…the female body is an ever-evolving landscape! Oftentimes the symptoms and their effects on women’s lives is underappreciated. After all, women comprise 49.6% of the world’s population, so nearly half of the world is going through it. Pelvic Floor Therapists have a unique perspective into the struggles of women throughout their lifespan and tend to be diligent in delineating between a condition or experience being “common” versus “normal”.
It is important to not confuse the two terms; just because something is common among a population of people, does not make it normal. It is common for women to have pain during their menstrual cycles and during pregnancy. It is common for women to struggle with returning to prior levels of function, including sexual function, following the birth of a child or with the journey of menopause. It is common for women to experience bladder leakage, and have difficulties with constipation. It is common for them to develop vaginal changes affecting personal relationships during and following menopause. But – is it normal?
Being intentional to support women throughout their lifespan and the journey their body makes along with them is important. Empowering women to pursue care proven to improve quality of life measures, throughout their lifespan, is imperative. Pelvic Floor Physical Therapy can be a tremendous tool allowing women to reclaim their bodies, and often their lives.
What Is Pelvic Rehabilitation?
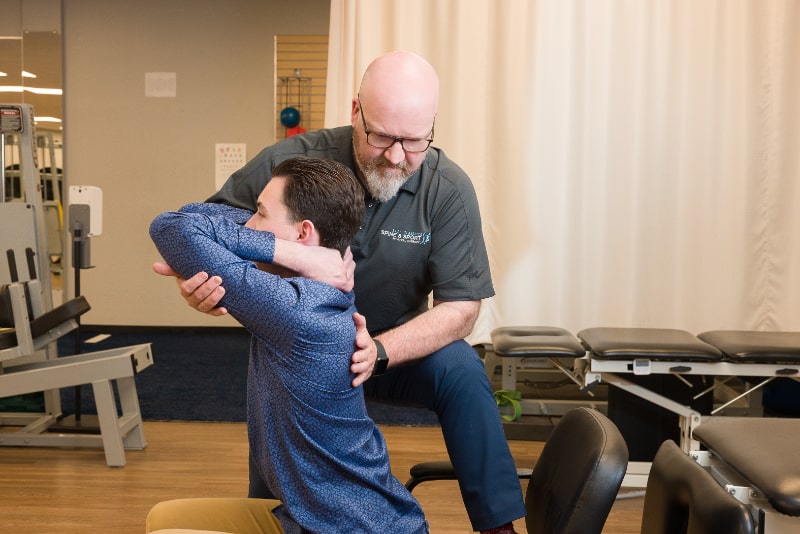
Pelvic floor rehab, or Pelvic Floor Physical Therapy, is treatment provided by a licensed Physical Therapist who has completed additional and specialized training for pelvic floor conditions. It involves an assessment of the low back, pelvis and hips, along with an external and internal pelvic examination. This examination is different from the one performed by a medical provider because it is assessing the “musculoskeletal” system; bones, joints, ligaments, and muscles.
Treating Women Through The Lifespan…
Experiencing the evolution from childhood to adulthood can be challenging for many children and adolescents. The development of new body parts, changes in appearance, acne and the beginning of menstruation can make this a very confusing time for kids. It’s difficult for parents too when the language has typically been “it’s normal to have pain during your period”. But what if your child is missing school, unable to attend social events, can’t tolerate tampon use, or is having severe acne? Pelvic floor therapy can be beneficial in assisting teens and parents to navigate these challenges and provide additional medical support when necessary.
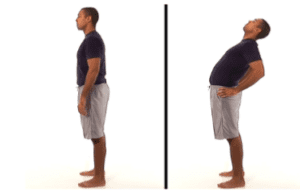
For adult women, the changes don’t stop there – there’s the journey of pregnancy and postpartum to consider as well. How do women handle the increasing demands of their bodies while making another human? Are they supposed to buy the lie that “pain is normal”? Or should they pursue additional care when their back, hips, and feet start to bother them with their advancing pregnancy? What about changes in bladder or bowel continence – when women start leaking are we really going to tell them that’s normal? Or when women aren’t able to resume previous activity, like running, strength training, or sexual relationships; do we accept that dysfunction as the new normal too? The short answer: Absolutely not.
Then there’s menopause, the final change. Menopause may bring new dysfunction; changes in vaginal and vulvar tissues, their robustness, pliability, and strength which can affect a woman’s ability to tolerate sexual relationships. There are changes that occur with new weight gain and the aches of an aging body. And then the misconception that these issues have been going on for “too long” and there’s “no helping them now”. The body is resilient! And it doesn’t matter if your urinary incontinence has been around since that first baby 30+ years ago, or if it just sprang up with the changes of menopause; pelvic floor rehab can still be beneficial.
Common conditions may include…
- Urinary Incontinence (Leakage)
- Urinary Frequency or Urgency
- Pain with Urination
- Bowel Incontinence (Smearing, or Gas)
- Pain with Bowel Movements
- Constipation
- Pelvic Organ Prolapse
- Pain with Vaginal Penetration (Dyspareunia)
- Painful Periods (Dysmenorrhea)
- Low Back/Pelvic Pain
- Menstrual Management
How Are We Treating It?
Pelvic floor rehab utilizes many treatment approaches including:
- Manual therapy: Soft tissue or muscle mobilization, joint mobilization, myofascial release
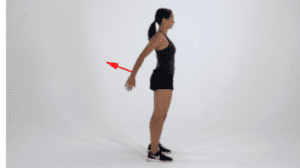
- Therapeutic exercise: Strengthening and flexibility interventions
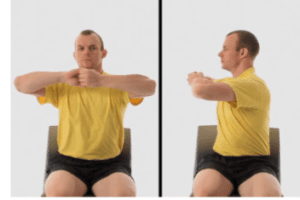
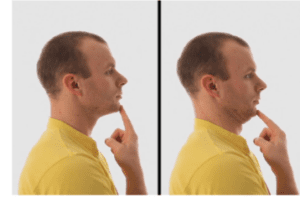
- Neuromuscular re-education: Teaching your muscles how to turn on/off appropriately and improving your awareness, coordination and control
- Therapeutic Activities: Helping you function within your specific life activities like lifting children or grandchildren, exercising and running, or being able to make it to the bathroom without leaking
What Does This Mean For You?
If you are struggling with any urinary (bladder), bowel, or reproductive/sexual health concerns, pelvic floor rehab may be appropriate and helpful for you. You do not have to live with your dysfunction, there is help – and Pelvic Floor Therapists are happy to join you in the journey.