Pelvic health physical therapists treat multiple disorders including urinary and fecal leakage, pelvic pain, urinary urgency and frequency, pelvic organ prolapse, diastasis recti, low back, hip and abdominal pain, pregnancy related pain and postpartum care, just to name a few. While our society has led us to believe that many of the mentioned problems are normal, know that there is conservative treatment available by visiting a pelvic floor physical therapist.
As a pelvic floor physical therapist I commonly have to ask deeper questions beyond our initial intake questionnaire that asks, “Do you ever leak urine when you laugh, cough, sneeze, exercise or jump?” as many circle “no.” After further questioning, however, a common reply is, “Well, yea, but I’ve had two children and my mom and grandma told me that’s simply a normal part of being a female” or, “I do, but only while running or jumping and a lot of my friends do too.” While this is a very common problem, there is conservative treatment for it…pelvic floor physical therapy! In fact, 25% of women have urinary incontinence and up to 50% of those have urinary leakage who exercise regularly. While most assume urinary leakage equates a weakness based problem, that is not always true and in some cases strengthening the pelvic floor can actually make urinary leakage worse! There are a variety of factors that may lead to urinary incontinence some of which include a weakened pelvic floor, overactive pelvic floor muscles that have a difficult time relaxing, damaged pelvic floor muscles resulting from surgical procedures or labor and delivery. Urinary leakage can also be caused by overactive and strong pelvic floor muscles in which the patient may be using mechanisms such as breath holding while lifting a heavy object, for example, as the increased pressure finds the weakest link within the system, commonly being the pelvic floor muscles. This is why having an evaluation by a pelvic floor physical therapist is so important to determine the contributing factors that are causing the leakage. These muscles need to be both strong in order to contract fully but also mobile to be able to relax fully to function appropriately. It is our job as pelvic floor physical therapists to train the pelvic floor muscles accordingly.
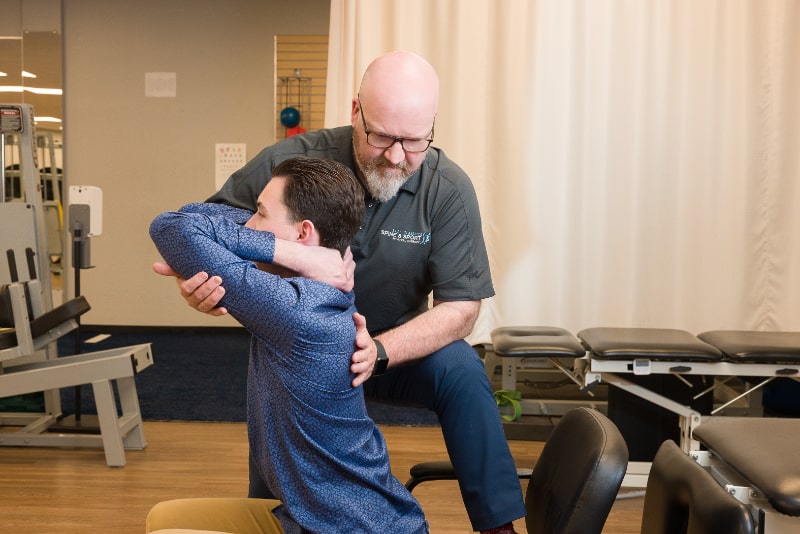
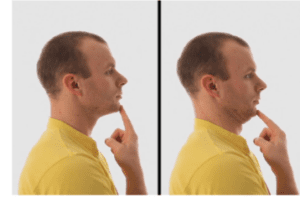
Another common disorder we treat is pelvic pain. Again, this is another common problem that many don’t feel comfortable talking about. 14.3% of women experience pelvic pain and often take years to tell their medical provider. There are many conditions that can lead to pelvic pain including cesarean sections, episiotomies, or complicated deliveries including the need of forceps, for example. Other diagnoses that commonly lead to pelvic pain include those such as interstitial cystitis (also known as painful bladder syndrome), endometriosis, past history of trauma/abuse, or chronic pelvic pain that has been occurring for 6 months or more without explainable cause. Pelvic pain can present differently such as sharp, stabbing pain or a deep, dull aching pain. Pelvic pain is not just limited to the pelvic area, however, as most also have discomfort in the surrounding area including the lower abdomen, hips and low back. Being orthopedically trained, we treat with an outward to inward approach meaning that we look at how the low back, the hips, core and the patient’s breathing mechanics are working first before examining the pelvic floor. Yes, even how you breathe plays a role in the function of the pelvic floor! With pelvic pain, it is common that the pelvic floor muscles spasm and are especially tight with a difficult time being able to relax. The pelvic floor muscles have to be able to relax in order to empty the bladder and bowels, so constipation and incomplete emptying of the bladder, or needing to strain in order to empty the bladder are commonly seen with pelvic pain. At Spine and Sport, we realize that pelvic pain can be a very sensitive topic to share. With your therapist being a female and having a private treatment room, it is our goal to make your comfort our priority. If you have any questions or concerns prior to your first visit, do not hesitate to call the office and your therapist will answer any questions you may have.
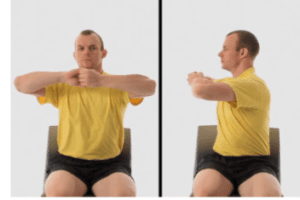
Pelvic floor physical therapists also commonly treat urinary urgency and frequency. These problems tend to have multi-faceted contributions. While there is typically a musculoskeletal involvement such as increased tone or trigger points within the pelvic floor muscles, there are typically other causes as well. One of which being dietary choices. There is a list of commonly known foods and fluids that contribute to bladder irritation. An abbreviated list includes coffee, tea, carbonation, citrus fruits, tomato based products and fruit juices. Additionally, not consuming enough water concentrates the urine which irritates the bladder. When the bladder becomes irritated, common side effects are urinary urgency and frequency. Your pelvic floor physical therapist may give you a bladder diary to complete for a few days to examine any possible foods or fluids that are contributing to your symptoms. Additionally, your physical therapist may have you work on something called behavioral retraining techniques if you report voiding more than 6-8 times or more than once every 2 hours within a 24 hour period. The bladder provides the brain with two signals. The first signal is sent to the brain when the bladder is about 25% full. This is a subconscious, warning signal to become alert of knowing where a nearby restroom is. This signal does not mean it is time to empty, though! The second signal to the brain is when it is truly time to empty the bladder due to being full. When patients use the restroom, “just in case” or more frequently than needed, this habit starts to trick the brain into feeling full before it actually is. Your pelvic floor physical therapist will educate you on behavioral retraining methods in order to prolong the time before voiding, thus being able to delay urinary urgency until that second signal tells your brain that the bladder needs to be emptied.
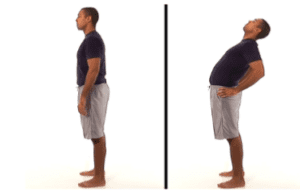
Pelvic organ prolapse is a condition that pelvic floor physical therapists commonly treat. The pelvic floor muscles are shaped like a bowl and one of their primary functions is to lift and support our organs. When the pelvic organs descend, this is pelvic organ prolapse. Pelvic organ prolapse is categorized by the specific organ and graded based on severity, or amount, of descent ranging from grade 1 (least amount of descent) to grade 4. Some common symptoms of this condition include a pressure or bulging sensation within the pelvis, a feeling as though “something is falling out” of the vagina, difficulty with inserting tampons, aching low back discomfort, urinary leakage or difficulty emptying the bladder or bowels. More often than not, patients report that their symptoms are aggravated by standing, walking or lifting heavy objects for prolonged time periods. While pelvic floor physical therapists are unable to change the grade of the prolapse that was given by the patient’s medical professional, there are many different interventions that can significantly reduce the severity of symptoms a patient may experience. Sometimes physical therapy care can completely eliminate pelvic organ prolapse symptoms! Your physical therapy may provide manual therapy, prescribe specific therapeutic exercises, and educate on how to breathe properly while performing strenuous activities to prevent breath holding among many other interventions.
This provides a very condensed list of the disorders a pelvic floor physical therapist treats. Our patients commonly experience low back, hip or abdominal pain, core weakness or diastasis recti after pregnancy. We treat pregnancy related pain and postpartum care including safe return to previous level of activity and proper body mechanics for the high demand that comes with being a new mother. If you have any questions about conditions we may treat as pelvic floor physical therapists, please do not hesitate to call any of our locations to speak with the therapist in order to determine if you are an appropriate candidate for pelvic health physical therapy.
To learn more about our pelvic health program, visit the Pelvic Health section on our website.
To request an appointment, click this link.